Oral Presentation Australian and New Zealand Pituitary Alliance 2025
Silent Corticotroph Tumours - Characteristics and Comparisons to Other Non-Functioning PitNETs: A Case Series (123424)
Background
Silent corticotroph adenomas (SCAs) are the second most common subtype of non-functioning pituitary neuroendocrine adenomas (NFPAs). They are ACTH- and T-PIT-positive on immunohistochemistry but lack biochemical hypercortisolism. SCAs are considered high-risk due to greater invasiveness, recurrence, and shorter progression-free survival1.
Aim
To compare demographics, clinical presentation, biochemistry, and imaging findings in patients with SCAs versus other NFPAs.
Methods
We retrospectively analysed patients with a pre-operative diagnosis of NFPA who underwent surgery at Macquarie University Hospital (2011–2025). Data included demographics, symptoms, tumour characteristics, and ACTH/cortisol levels pre- and post-operatively.
Results
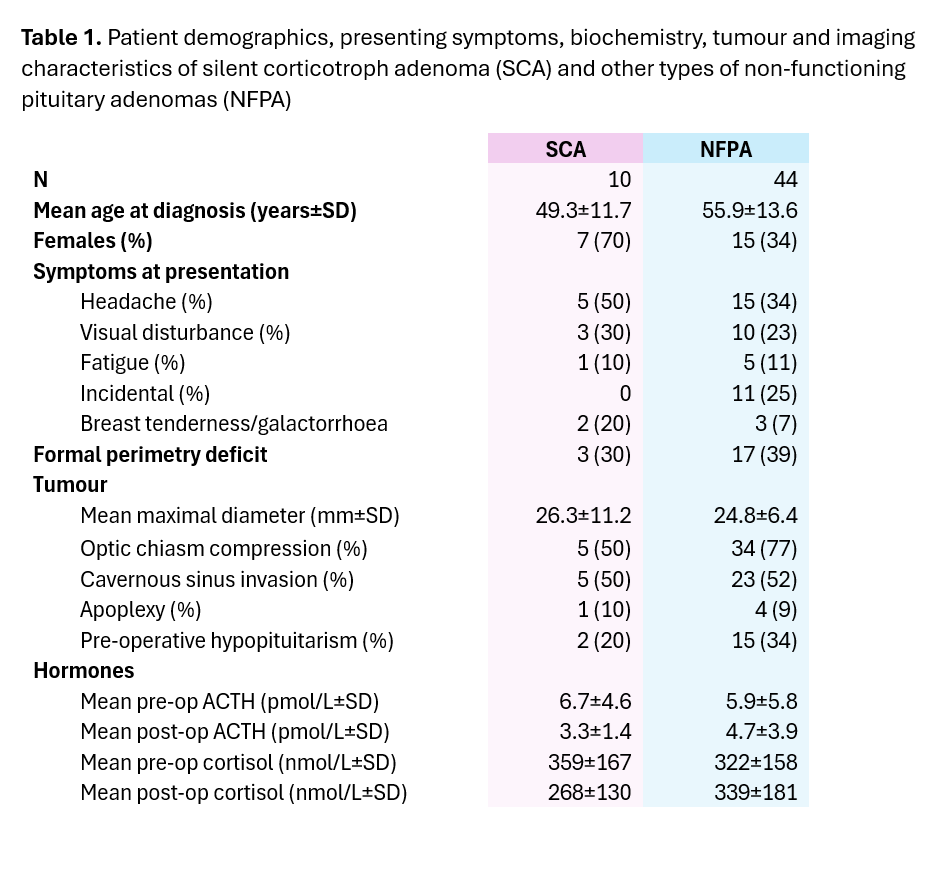
Among 54 patients, 10 had SCAs (Table 1). The most common non-SCA NFPAs were gonadotropinomas (61%), plurihormonal (14%), and null cell adenomas (14%) [Table 1]. All SCAs were macroadenomas and ACTH-positive; 3/10 were T-PIT positive (pending full review). Patients with SCAs were younger (mean age 49.3 vs 55.2 years) and more often female (70% vs 34%). Headaches (50% vs 34%), visual symptoms (30% vs 23%), and galactorrhoea (20% vs 7%) were more frequent in SCAs. Mean tumour size was slightly larger (26.3 mm vs 24.8 mm). No significant differences were seen in pituitary apoplexy (10% vs 9%) or cavernous sinus invasion (50% vs 52%). Mean pre-operative ACTH and cortisol in SCAs were 6.7 pmol/L and 359 nmol/L, decreasing post-operatively to 3.3 pmol/L and 268 nmol/L.
Conclusion
SCAs tend to occur in younger, predominantly female patients, and are associated with larger tumours and more frequent symptoms, though tumour aggressiveness is similar to other NFPAs at time of surgery. Post-operative ACTH may support imaging in recurrence monitoring. Close follow-up remains essential given their high-risk profile.